




Root canal therapy is one of the most common dental procedures performed, with over 14 million procedures completed each year. “Endo” is the Greek word for inside, and “dont” is the Greek word for tooth. Thus, endodontics refers to the treatment of the inside of the tooth. A root canal therapy is the most common endodontic procedure.
The dental pulp is the soft tissue in the center of the tooth which contains the blood and nerve supply for the tooth. It enters the tooth from the bottom of the root(s) and extends to the center of the tooth through small canals. In health, the dental pulp supplies the tooth with temperature sensation and is responsible for the continued development of the root structure. When damaged, the dental pulp often causes pain that is felt as a tooth ache or temperature sensitivity. If the inflammation or infection in the dental pulp progresses, it can cause damage to the jawbone that supports the tooth. At this stage, the tooth is usually sore to chewing, and an abscess may form at the base of the root.
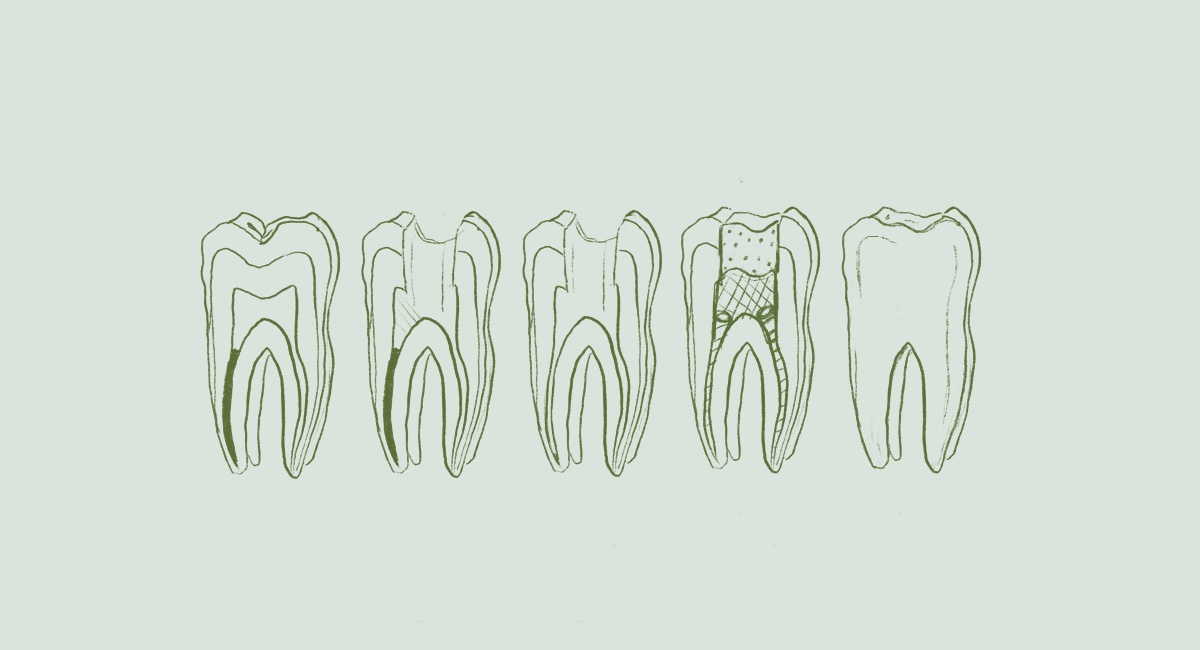
The procedure that restores the tooth and jawbone and allows the tooth to function normally is called a root canal procedure, often referred to as a “root canal”. The purpose of a root canal procedure is to remove any inflamed or infected dental pulp tissue, disinfect the inside of the tooth, and seal the root canals so that future infection is not possible. The typical root canal involves making a small access hole into the top of the tooth, which allows the endodontist to work inside the root canal space and preserve as much natural tooth as possible. Once completed, success rates are very high for root canal therapy and the tooth should last a lifetime if properly restored and maintained.
For more information on root canal therapy, please visit the American Association of Endodontists.
Endodontic retreatment is the name of the procedure to address problems in the root canal space on a tooth that has already undergone root canal therapy. While initial root canal therapy should last a lifetime, several reasons exist for failure after a root canal treatment. Common reasons for failure include:
Identification of the reason for failure is essential to being able to correct the problem. With proper diagnosis, a root canal retreatment can often be completed which will give the natural tooth a second chance. Retreatment involves carefully removing the existing root canal filling materials within the tooth, cleaning and disinfecting the canal system, and refilling the root canal space. Success rates are high when the problem is identified and corrected. As with an initial root canal procedure, proper placement of a permanent filling or crown is essential for success of the treatment.
For more information on endodontic retreatment, please visit the American Association of Endodontists.
Often referred to as an apicoectomy, endodontic surgery is a procedure to treat the end of the roots to prevent or treat inflammation or infection in the jawbone. An apicoectomy is most commonly completed after all other options have been exhausted to save the tooth. Many teeth that undergo an apicoectomy have had an initial root canal treatment that was not able to fix the problem, or a new problem occurred that compromised the tooth.
An apicoectomy is performed by removing the tip of the tooth root. To access the tip of the root, a small incision is made into the gum tissue and the jawbone that covers the root is exposed and carefully removed. Any infection present in the jaw bone is removed and cleaned. Once the root tip is visible, it is thoroughly checked for fractures which could impact the long term support of the tooth. Approximately 3mm of root tip is removed and a bioceramic filling is placed at the end of the root to seal the root canal space. The gum tissue is closed with sutures and the jawbone often fills in around the end of the root where the infection was present and restores function and stability to the tooth.
For more information on endodontic surgery, please visit the American Association of Endodontists.
Cracks and fractures are common problems that affect our teeth. Cracks are generally formed when a tooth is asked to function harder than it is designed to function. Over time, small cracks can spread and lead to larger cracks deep enough to reach the root canal space. Fractures are generally caused by trauma to a tooth. Car accidents, bike stunts gone wrong, and trips and falls are common ways to fracture a tooth. If a fracture is deep enough to reach the pulp space, endodontic treatment is necessary to save the tooth. The key to successful treatment for cracks and fractures involves an accurate diagnosis and an understanding of how deep the damage has progressed. Shallow cracks and fractures are often treatable with a root canal procedure. Deep cracks and fractures often require extraction of the tooth. Endodontists use equipment and procedures that can help diagnose and determine the depth of a crack or fracture, so that the proper treatment can be completed to return your smile to health.
For more information on cracked teeth, please visit the American Association of Endodontists.
For more information on fractured teeth, please visit the American Association of Endodontists.
Root canals are the small passageways from the jawbone to the center of your tooth which contain the blood and nerve supply (dental pulp) for your tooth. When the root canal space becomes infected or damaged, it can cause damage to the jawbone that supports the tooth. To fix the problem, a root canal procedure is performed. During this procedure, the canals that exist within the tooth are cleaned, disinfected, and sealed to prevent future problems or infection.
Root canal treatment is needed when the root canal system becomes damaged. Common problems that may lead to root canal damage are cavities, fractures, cracks, and trauma. It is important to identify the reason a root canal treatment is necessary to properly treat the condition.
Endodontists are specialists whose practice is limited to the treatment and prevention of diseases related to the root canal system and the supporting jawbone. Less than three percent of dentists are specialized in endodontics. Every endodontist has completed dental school and a residency program specialized in endodontics. A board-certified endodontist has completed an additional multi-year vetting process by the American Board of Endodontists which certifies that they are an expert in the field of endodontics. Board certified endodontists have achieved the highest degree of training and specialization in their field.
In general, a root canal procedure should be no different than having a filling or a crown placed. Our office uses advanced anesthesia practices to ensure that the area we are working on is numb before starting our work. Most patients are surprised at how painless the procedure feels.
Every patient and tooth are different, but in general, root canal treatments are usually completed in one visit within 45 minutes to an hour. Depending on the situation, some teeth require the treatment to be completed in multiple visits. If this is the case, we will place a temporary filling in the tooth until you can return to complete the treatment.
While extraction is always an option, it is often not the best option. Endodontists are trained to save the natural set of teeth when possible and have special skills and equipment to accomplish that task. Saving a natural tooth often results in a more natural appearance and a more functional mouth. In addition, saving a natural tooth is often less expensive and less time consuming than removing and replacing a tooth. At your visit, we will discuss all the options available and choose an option that fits your individual needs and desires.
On the day of treatment, follow your normal routine until your appointment time. Eating and drinking is allowed before the root canal procedure, and it is not advised to show up on an empty stomach. Wear comfortable clothing and plan to lay back in the dental chair for about an hour.
Every procedure starts with an exam to determine what treatment is required. Any required X-rays will be made, and we will explain any findings. We will ask about your symptoms and perform a thorough exam of the problem area. Treatment options and fees will be presented, and you will have a chance to ask all the questions you may have.
After numbing the area with local anesthetic, and checking to make sure you are completely numb, we will begin the procedure. A rubber dam will be used during the entire root canal procedure. We will ensure it is as comfortable as possible. During treatment, the doctor and assistant will work as a team while working through a high-powered microscope to complete the procedure. Expect the procedure to last approximately 45 minutes to one hour and fifteen minutes depending on the tooth. The procedure should be painless, and we will take every step to keep you comfortable. If you ever experience discomfort, please let us know immediately.
After the root canal procedure is complete, a temporary filling will be placed in the tooth unless your dentist has asked us to place a permanent filling. It is very important to avoid chewing hard or sticky food while a temporary filling is in place. Please call your dentist right away to schedule an appointment for the permanent filling.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. Over-the-counter medications, such as Advil® or Tylenol®, are usually enough to manage this sensitivity. In some cases, prescription medications may be necessary and are available from your endodontist. Your tooth may continue to feel slightly different from your other teeth for some time after your endodontic treatment is completed. This is normal and usually resolves completely over time. Of course, if you experience pressure or pain that lasts more than a few days or becomes severe, please call our office.
Avoid chewing on the tooth for the first few days, if possible, which will help alleviate any discomfort with the tooth during the healing process. If a temporary filling was placed, do not chew anything hard or sticky with the tooth until a permanent filling or crown has been placed by your dentist. In the rare case that your temporary filling is lost before you have the tooth permanently filled, please call our office.
Our office accepts all PPO dental insurance plans. We are an Out-of-Network provider, meaning we are not contracted, or, In-Network with any insurance company. We do not accept Medicare, Medicaid, or HMO dental plans.
Please remember that you are fully responsible for all fees charged by this office regardless of your insurance coverage. Although we are not a party to the contractual agreement with your insurance company, we do want to help you receive the maximum reimbursement to which you are entitled. As a courtesy, we will submit all claims to your insurance company on your behalf.
At all times, you can be confident that we will always provide you with our best services using the newest and best technology to improve your treatment outcomes regardless of whether you have insurance coverage.
Please also note that our office is a fee-for-service practice. This means that our patients pay upfront, in full, for their dental care at time of service. As a courtesy, we will submit all claims to your insurance company on your behalf and you will be reimbursed directly by your insurance company.
Our office works with a number of partners to offer financing options for our patients: Care Credit, Sunbit, Cherry. All options allow you to finance your treatment, interest-free. Sunbit and Cherry require no hard credit check. All major credit cards are accepted.
If you have questions about our financial policy or wish for our office to provide you with an estimate prior to your appointment, please call our office at (605) 961-9092.